Volume 7, Issue 4 (December 2022)
J Environ Health Sustain Dev 2022, 7(4): 1777-1796 |
Back to browse issues page
Download citation:
BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:



BibTeX | RIS | EndNote | Medlars | ProCite | Reference Manager | RefWorks
Send citation to:
Thomas J, Parameswaran M. Impact of Climate and Pollution on Schizophrenia: A Narrative on Exposure-Response Relationship. J Environ Health Sustain Dev 2022; 7 (4) :1777-1796
URL: http://jehsd.ssu.ac.ir/article-1-530-en.html
URL: http://jehsd.ssu.ac.ir/article-1-530-en.html
Big Data analytics Lab, School of Computer Science, Presidency University, Bangalore, India.
Full-Text [PDF 892 kb]
(185 Downloads)
| Abstract (HTML) (424 Views)
.PNG)
Figure 1: Methodology used in this study
Mathematical models
Multiple linear regression models can be used to examine mental health emergency cases as the dependent variable and pollution exposure as the predictor variable(s)19,23,24. The use of a traditional method with exposure variables as mean temperature or PM2.5 or any other significant pollutant in a city was expressed as follows.
Where HA is the number of hospital admissions, X is the mean of a climate variable, and e is a random error with a mean of 0. As a result, μ denotes the background rate, and α denotes the difference in rate for increased pollution in a city. The data were analysed using multiple variable techniques and a sequence of variables to characterize the exposure status; each variable represented a different pollution variable. To forecast hospital admissions, p was considered an independent factor. The model was as follows.
HA=β0X0 + β1X1 + β2X2 +……+e (Eq. 2)
Where, Xj is the proportion of pollutants. The impact of a single exposure event is not always limited to the time frame in which it is detected, but can also be postponed. This poses the question of how to represent the relationship between a single exposure event and a sequence of subsequent outcomes, as well as describe the distribution of effects in various periods following the event (lags). Finally, this phase necessitates the emergence of a new lag dimension in an exposure-response connection, which describes the spatial pattern of the effect. A time-series Poisson regression analysis may be used to look at the links between short-term air quality and outpatient visits for schizophrenia with varying lag days. The average daily exposure levels of contaminants were calculated using hourly data from the stations. The major benefit of this technique is that it allows the model to include a thorough description of the exposure-response relationship time course, which allows for a complete effect evaluation in the event of delayed contributions. To characterize the time series of outcomes Yt, a generic model25 representation is used with t = 1,..., n. The results of time series studies of environmental variables are often counted daily, which are believed to come from an excessively scattered Poisson distribution.
ω ≡ E(Y) (Eq. 3)
Where, Y is intended to originate from an exponential family distribution and S is a monotonic link function.
S(ωt)=α
The parameter vectors provide the smoothed connections between the variables xti and the linear predictor βi are represented by the functions pi. The related coefficients γj in the variables
A Poisson generalized regression analysis combined with a distributed lag non-linear model (DLNM) was used in various research to investigate the influence of meteorological variables on schizophrenia admissions18,26. The DLNM is a paradigm for modelling non-linear exposure-response connections as well as delayed effects concurrently. Admissions information, including age, gender, home address, birth month, and marital status, can be gathered from hospitalized patients with abrupt onset of schizophrenia. A research applying this technique is for analyzing the relationship between daily Diurnal temperature range (DTR) and schizophrenia data26. DTR was calculated using the maximum temperature minus the lowest temperature on the same day. Daily climatic variables such as mean temperature, maximum, and minimum temperature, humidity levels, wind speed, and rainfall can be confounding factors18. The association between short-term air quality and schizophrenia outpatient visits with various lag days was investigated using a time series Poisson regression model. Concentrations of PM10, SO2, and NO2, as well as the daily mean humidity levels and average temperature, allow modifying the possible impact of weather on hospital admissions27.
E (Yβ) represents the reported daily number of hospital admissions on day t, as well as the coefficients between pollutants and hospital admissions respectively, ns is a date-time natural cubic spline function; St is the daily average of air pollutants on day t; D means the day of the week; 3 is degrees of freedom (df) used for time and humidity (H); 6 is df used for average temperature (T) and b is the intercept. When this core model is created, it is used by inserting air pollution concentrations into a single-pollutant model, researchers can look into the link between schizophrenia admissions and air pollution. Several lag patterns were incorporated as sensitivity tests in the core models since health effects might last for several days. Single-day delays and moving average lags (lag 1 to lag 3) can be used to assess the delayed consequences of pollutants. Two-pollutant models can be considered for examining the stability of effects after adjusting for co-pollutants.
Data sources and software tools of the study
Time series environmental data can be obtained across a wide variety of resources; from mobile phone sensors to more sophisticated monitoring tools and databases operated by state, federal agencies, and organizations. Many researchers examined data sets from online outlets, such as Kaggle. The temperature variables can be collected from the respective country's Bureau of Meteorology, including relative humidity, rainfall, atmospheric pressure, and wind directions. Satellite data may be available to measure green space. A data collection from the Landsat program for Denmark is available28. The authors used Danish national registers providing information on all people living in Denmark to examine traffic-related exposures that influence schizophrenia risk29,30. Standard Model Instrumentation for Noise Assessments (STAMINA) can be used for estimating residential traffic noise levels31. In India, pollution data can be collected from the Central Pollution Control Board (CPCB). All major air pollutants and noise quality data are freely available on official websites. India Meteorological Department (https://mausam.imd.gov.in) will provide all kinds of climate data for researchers. The Automated Meteorological Data Acquisition System of Japan can collect weather data from meteorological satellites containing altitude, location, and temporal information32.
The major source of psychiatric data in this research is emergency admission statistics from hospitals33. Another important source is patient data from insurance companies. Some studies analyzed daily data of outpatient admissions. The data from a teenage national well-being study in the Netherlands, including psychiatric trauma questions focused on the Kessler 10 scale31. In quantifying psychiatric illness, parent assessment tools and sub-scale scores of anxiety, depressive symptoms, somatic symptoms, and withdrawal scales using the behavior assessment system for children (BASC) are suitable19. Symptom-Checklist-90-Revised Scale (SCL-90-R) can be considered for life transition stress and cognitive stress assessment34. The National Morbidity, Mortality, and Air Pollution Study (NMMAPS) data set is accessible to the public via the Internet-based Health and Air Pollution Surveillance System website. It contains 5114 observations of daily mortality as well as meteorological and pollution information for Chicago.
The DLNM kit inside the R statistical environment includes a range of tools to define and analyze the effects of lag. This structure is introduced in the 'DLNM' R bundle, which offers functions to execute a wide variety of models within the DLNM family, with a focus on graphs, and emphasis on graphical representation2. Most statistical studies of the problem mentioned were carried out using R tools with the following packages (version 4.1.3): 'mgcv', 'nlme', data.table, Hmisc, landsat, lubridate, plyr, raster rgdal, RStoolbox, sp28,35,36. Statistical analysis can be done by Stata17, WEKA version 3.9.6, and SAS version 9.4 software23,24 .
Table 1: Summary table of papers that used different regression methods
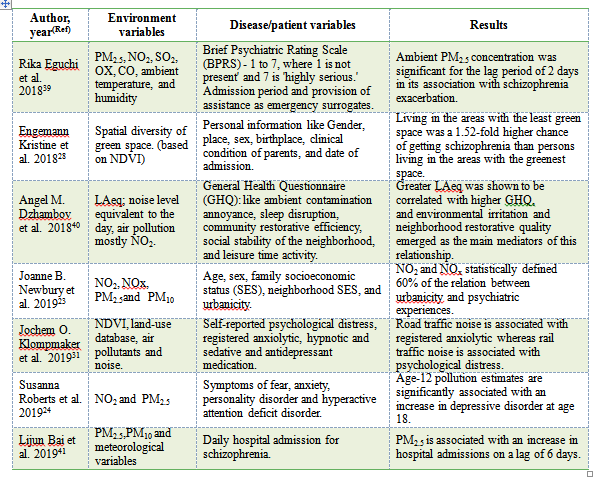
The relationship between particulate matter (PM) and the severity of mental health have been investigated in many papers using a wide range of regression techniques or its combination. Major classifications are logistic regression and linear regression. Time-series Poisson regression model is most common in these types of studies. Eguchi39 used multivariate logistic regression and determined that ambient PM2.5 concentration was associated with the exacerbation of schizophrenia. Pedersen et al. found that geographical distance from residence to the nearest major road had a significant effect on schizophrenia. The highest risk was found in children living 500–1000 meters from the nearest major road42. Liang27 found that short-term air pollutants, such as PM10, SO2, and NO2 exposure might contribute to the increased risk of outpatient visits for schizophrenia. Even though there is no universal supremacy of one technique, regression techniques have been widely used for this problem. There was a finding that hospital admissions increased with increasing levels of PM2.5 during the summer, which was analyzed using Poisson regression techniques43. The relationships between the PM and the hospital admission for schizophrenia were assessed using a time-series Poisson regression model with the duration of hospital admission as the relevant variable41. In several lag models, the strongest correlations were seen on the sixth day. Increased likelihood of hospital admissions for schizophrenia was linked to PM air pollution, with greater relationships among married and female patients. This result is not in line with other researchers' findings.
Table 2: Summary of papers using Pearson and Spearman correlations

To analyze mental illness and environmental factors, apriori algorithm is rarely used. Given that the data analysis techniques are not limited to the above-mentioned methods, depending on the problem and type of data sets, a researcher may get more choices. For example, an analysis of the correlation between sub-group characteristics like age, gender, marital status, and employment status, may need algorithms of deep neural networks49.
.PNG)
Figure 3: Correlation of PM2.5, PM10, Temp, and CO with NoA in Bangalore city
.PNG)
Figure 4: Lag-specific effects with NoA in terms of RR
Full-Text: (154 Views)
Impact of Climate and Pollution on Schizophrenia: A Narrative on Exposure-Response Relationship
Jobin Thomas 1*, Murali Parameswaran 1
1 Big Data analytics Lab, School of Computer Science, Presidency University, Bangalore, India.
Jobin Thomas 1*, Murali Parameswaran 1
1 Big Data analytics Lab, School of Computer Science, Presidency University, Bangalore, India.
| A R T I C L E I N F O | ABSTRACT | |
| NARRATIVE REVIEW | Introduction: In recent years, the relationship between environment and psychological well-being has been paid attention among researchers. With the preceding emphasis on climate change, significant studies have been conducted to analyze the relationship between air pollutants, such as nitrogen dioxide (NO2), sulfur dioxide (SO2), oxidants (OX), carbon monoxide (CO), particulate matter (PM) of size ≤ 2.5 µm (PM2.5), and atmospheric factors like surrounding temperature, relative humidity, and their impact on health, especially mental health. Materials and Methods: This narrative review was conducted on the exposure-response relationship between environmental factors and air pollutants, and one type of mental health challenge, schizophrenia. Accordingly, the data analysis techniques applied to this problem were reviewed. The key research elements considered from existing studies included the relation between air quality and mental health, mathematical models, data sources, and areas that remain unexplored. Results: It was observed that most studies related to the environmental impact on schizophrenia have been limited to temperature and few pollutants. Conclusion: In the primary feasibility study, PM2.5, PM10, and temperature had a positive correlation and lag effect with the daily number of emergency admissions of schizophrenia. |
|
Article History: Received: 27 September 2022 Accepted: 20 November 2022 |
||
*Corresponding Author: Jobin Thomas Email: jobinthomas@presidencyuniversity.in Tel: +91 906157-9191 |
||
Keywords: Temperature, Climate Change, Mental Health, Schizophrenia, Air Pollution. |
Citation: Thomas J, Parameswaran M. Impact of Climate and Pollution on Schizophrenia: A narrative on Exposure-Response Relationship. J Environ Health Sustain Dev. 2022; 7(4): 1777-96.
Introduction
Concerns about global warming have increased in recent years, especially with the various alarming reports from the Intergovernmental Panel on Climate Change (IPCC)1. Determining the impact of climate variables on health issues has gained more attention2,3. Recent studies have focused on the effect of external factors on mental health4,5,6. Schizophrenia is one of the major mental health issues affecting the quality of life7,8 and it is difficult to diagnose. Positive symptoms (delusions and hallucinations), negative symptoms (reduced motivation, reduction in spontaneous speech, and social disengagement), and cognitive impairment are the features of schizophrenia9. The incidence of schizophrenia can only be confirmed by a medical practitioner. One of the easiest ways to analyze the incidence of schizophrenia is by exploring hospital admission information10, either the in-patient information or the casualty admission information11. The relation between climate change or air pollution and schizophrenia has received a lot of attention in recent years12. Several meteorological potential causes have been identified for schizophrenia5,13. A variety of climatic conditions may have a role in the formation of psychosis in schizophrenia patients14 and potentially increase their admission rates to psychiatric facilities15. According to a meta-analysis of twins with schizophrenia, the heredity of schizophrenia is substantial, and there are minor but significant common environmental factors affecting the chance of developing schizophrenia16.
In the application of data mining methods to pollution health analysis, a survey was conducted distinguishing the current patterns, challenges, data sources, and new directions to explore and data analysis was used in the study of disease transmission in air pollution. Climate data and pollution data have been separately collected by various agencies for a long time. For instance, temperature data for Bangalore city has been available since 190117. The highest temperature, lowest temperature, maximum humidity, minimal humidity, maximum pressure, and minimum pressure were considered as climate factors. Air pollutants include the particulate matter of size ≤ 10 µm (PM10), particulate matter of size ≤ 2.5 µm (PM2.5), sulfur dioxide (SO2), nitrogen dioxide (NO2), nitrogen oxides (Nox), and ammonia (NH3), lead (Pb). Day and night noise quality and normalized difference vegetation index (NDVI) were also considered. Because of the quality of the results, future studies need to analyze variables such as illness duration, medication history, smoking habits, employment, indoor noise exposure (e.g., from neighbors), and place of birth. The environmental data, usually derived from meteorological agencies or environmental agencies, is well established and easily available even on an hourly or daily timescale.
The time series data of pollutants and climate variables are huge in quantity and easily available. However, schizophrenia data is minimal and difficult to access because of the nature of medical data and the non-availability of digitized content in developing nations. The hospital data is sparse and sporadic, especially in developing or underdeveloped countries, digital records may not be adequately maintained, or the datasets may be bound by other constraints resulting in lots of missing values. One of the key motivations for pursuing this problem is the use of two kinds of time series data with such drastically different natures. The environmental impact of a disease may have a delay of a few days before the onset of the disease. This lag effect is observed in hospital admission in some of the studies18,19. The lag effect is interesting in its own right. The present study aims to explore the nature of lag effects across multiple environmental and pollution parameters, as well as the techniques that might be relevant for identifying and incorporating the lag effect for predicting hospital admissions.
In India (2017), 197.3 million people were suffering from mental illnesses or 14% of the national population and 4.7% of the total disability-adjusted life years (DALYs) were attributable to mental disorders, compared to 2.5% in 199020 (Indian Council of Medical Research Public Health Foundation). With the expected improvement in healthcare facilities, more patients may start availing of the facilities. It is also expected that more patients will break past taboos and refer for diagnosis and treatment of mental illnesses. With this change in societal approach, the problem of the availability of data may mutate into the problem of not fully utilizing the data which is much better than dealing with sparse data. The other aspect the study aims to find is based on to what extent can existing technology be used to speed up transitions in mental health. Hospital capacity is one of the key factors for effectively mitigating any health issue. Health officials can increase the capacity on demand if they have some clue regarding a likely increase in the number of patients, as has been evidenced by the efforts of all governments during the recent COVID-19 outbreak. Moreover, techniques that can help psychiatric health officials were explored to decide whether there is a need to improve hospital capacity.
The lack of uniformity of results across multiple geographical regions was the key concern in this review. It is known that every region or country has its environmental diversity. For instance, the climate of Bangalore, India is atypical for a city in a tropical zone. The study checked the feasibility of exploring the relationship between environmental variables and schizophrenia, especially in India. However, the impact of the environment on the severity of schizophrenia symptoms was not well understood13,18,21,22 and the biological mechanism behind did not belong to the scope of this study. The literature based on the techniques used to analyze the relationship between schizophrenia and environmental factors was reviewed.
Concerns about global warming have increased in recent years, especially with the various alarming reports from the Intergovernmental Panel on Climate Change (IPCC)1. Determining the impact of climate variables on health issues has gained more attention2,3. Recent studies have focused on the effect of external factors on mental health4,5,6. Schizophrenia is one of the major mental health issues affecting the quality of life7,8 and it is difficult to diagnose. Positive symptoms (delusions and hallucinations), negative symptoms (reduced motivation, reduction in spontaneous speech, and social disengagement), and cognitive impairment are the features of schizophrenia9. The incidence of schizophrenia can only be confirmed by a medical practitioner. One of the easiest ways to analyze the incidence of schizophrenia is by exploring hospital admission information10, either the in-patient information or the casualty admission information11. The relation between climate change or air pollution and schizophrenia has received a lot of attention in recent years12. Several meteorological potential causes have been identified for schizophrenia5,13. A variety of climatic conditions may have a role in the formation of psychosis in schizophrenia patients14 and potentially increase their admission rates to psychiatric facilities15. According to a meta-analysis of twins with schizophrenia, the heredity of schizophrenia is substantial, and there are minor but significant common environmental factors affecting the chance of developing schizophrenia16.
In the application of data mining methods to pollution health analysis, a survey was conducted distinguishing the current patterns, challenges, data sources, and new directions to explore and data analysis was used in the study of disease transmission in air pollution. Climate data and pollution data have been separately collected by various agencies for a long time. For instance, temperature data for Bangalore city has been available since 190117. The highest temperature, lowest temperature, maximum humidity, minimal humidity, maximum pressure, and minimum pressure were considered as climate factors. Air pollutants include the particulate matter of size ≤ 10 µm (PM10), particulate matter of size ≤ 2.5 µm (PM2.5), sulfur dioxide (SO2), nitrogen dioxide (NO2), nitrogen oxides (Nox), and ammonia (NH3), lead (Pb). Day and night noise quality and normalized difference vegetation index (NDVI) were also considered. Because of the quality of the results, future studies need to analyze variables such as illness duration, medication history, smoking habits, employment, indoor noise exposure (e.g., from neighbors), and place of birth. The environmental data, usually derived from meteorological agencies or environmental agencies, is well established and easily available even on an hourly or daily timescale.
The time series data of pollutants and climate variables are huge in quantity and easily available. However, schizophrenia data is minimal and difficult to access because of the nature of medical data and the non-availability of digitized content in developing nations. The hospital data is sparse and sporadic, especially in developing or underdeveloped countries, digital records may not be adequately maintained, or the datasets may be bound by other constraints resulting in lots of missing values. One of the key motivations for pursuing this problem is the use of two kinds of time series data with such drastically different natures. The environmental impact of a disease may have a delay of a few days before the onset of the disease. This lag effect is observed in hospital admission in some of the studies18,19. The lag effect is interesting in its own right. The present study aims to explore the nature of lag effects across multiple environmental and pollution parameters, as well as the techniques that might be relevant for identifying and incorporating the lag effect for predicting hospital admissions.
In India (2017), 197.3 million people were suffering from mental illnesses or 14% of the national population and 4.7% of the total disability-adjusted life years (DALYs) were attributable to mental disorders, compared to 2.5% in 199020 (Indian Council of Medical Research Public Health Foundation). With the expected improvement in healthcare facilities, more patients may start availing of the facilities. It is also expected that more patients will break past taboos and refer for diagnosis and treatment of mental illnesses. With this change in societal approach, the problem of the availability of data may mutate into the problem of not fully utilizing the data which is much better than dealing with sparse data. The other aspect the study aims to find is based on to what extent can existing technology be used to speed up transitions in mental health. Hospital capacity is one of the key factors for effectively mitigating any health issue. Health officials can increase the capacity on demand if they have some clue regarding a likely increase in the number of patients, as has been evidenced by the efforts of all governments during the recent COVID-19 outbreak. Moreover, techniques that can help psychiatric health officials were explored to decide whether there is a need to improve hospital capacity.
The lack of uniformity of results across multiple geographical regions was the key concern in this review. It is known that every region or country has its environmental diversity. For instance, the climate of Bangalore, India is atypical for a city in a tropical zone. The study checked the feasibility of exploring the relationship between environmental variables and schizophrenia, especially in India. However, the impact of the environment on the severity of schizophrenia symptoms was not well understood13,18,21,22 and the biological mechanism behind did not belong to the scope of this study. The literature based on the techniques used to analyze the relationship between schizophrenia and environmental factors was reviewed.
Materials and Methods
The articles were selected from Elsevier, Springer, InderScience, and IEEE databases. Around 120 research papers culminated in the search queries. The fine-grained inquiry used the inclusion and exclusion criteria to minimize the number of papers around 70. The articles were obtained from a three-part search procedure. The search keywords included ("machine learning") AND ((environment AND mental health) OR (exposure)), ("machine learning") AND ((pollution AND schizophrenia) OR (exposure)), ("data mining") AND ((environment AND health) OR (exposure)). The studies were classified based on major techniques applied and based on the impact of pollution on schizophrenia. Literature consisting of both schizophrenia-specific papers and related domains in mental health was analyzed. The study methodology is plotted in Figure 1. The researchers attempted to visualize these problems as regression, correlation, and lag-based techniques. A holistic classification of techniques applied is provided in Figure 2. They were discussed in detail in the following subsections.
In this paper, the key questions considered are:
Q1: About air quality and mental health, to what extent has data mining been applied?
Q2: What would be a suitable data set?
Q3: What fruitful directions remain unexplored?
The above questions are discussed in the following sections. The studies were sorted and classified based on techniques applied to the environmental impact of mental health, and various attributes and reviews were included to generate the classification..PNG)
Figure 1: Methodology used in this study
Mathematical models
Multiple linear regression models can be used to examine mental health emergency cases as the dependent variable and pollution exposure as the predictor variable(s)19,23,24. The use of a traditional method with exposure variables as mean temperature or PM2.5 or any other significant pollutant in a city was expressed as follows.
Where HA is the number of hospital admissions, X is the mean of a climate variable, and e is a random error with a mean of 0. As a result, μ denotes the background rate, and α denotes the difference in rate for increased pollution in a city. The data were analysed using multiple variable techniques and a sequence of variables to characterize the exposure status; each variable represented a different pollution variable. To forecast hospital admissions, p was considered an independent factor. The model was as follows.
HA=β0X0 + β1X1 + β2X2 +……+e (Eq. 2)
Where, Xj is the proportion of pollutants. The impact of a single exposure event is not always limited to the time frame in which it is detected, but can also be postponed. This poses the question of how to represent the relationship between a single exposure event and a sequence of subsequent outcomes, as well as describe the distribution of effects in various periods following the event (lags). Finally, this phase necessitates the emergence of a new lag dimension in an exposure-response connection, which describes the spatial pattern of the effect. A time-series Poisson regression analysis may be used to look at the links between short-term air quality and outpatient visits for schizophrenia with varying lag days. The average daily exposure levels of contaminants were calculated using hourly data from the stations. The major benefit of this technique is that it allows the model to include a thorough description of the exposure-response relationship time course, which allows for a complete effect evaluation in the event of delayed contributions. To characterize the time series of outcomes Yt, a generic model25 representation is used with t = 1,..., n. The results of time series studies of environmental variables are often counted daily, which are believed to come from an excessively scattered Poisson distribution.
ω ≡ E(Y) (Eq. 3)
Where, Y is intended to originate from an exponential family distribution and S is a monotonic link function.
S(ωt)=α
The parameter vectors provide the smoothed connections between the variables xti and the linear predictor βi are represented by the functions pi. The related coefficients γj in the variables
A Poisson generalized regression analysis combined with a distributed lag non-linear model (DLNM) was used in various research to investigate the influence of meteorological variables on schizophrenia admissions18,26. The DLNM is a paradigm for modelling non-linear exposure-response connections as well as delayed effects concurrently. Admissions information, including age, gender, home address, birth month, and marital status, can be gathered from hospitalized patients with abrupt onset of schizophrenia. A research applying this technique is for analyzing the relationship between daily Diurnal temperature range (DTR) and schizophrenia data26. DTR was calculated using the maximum temperature minus the lowest temperature on the same day. Daily climatic variables such as mean temperature, maximum, and minimum temperature, humidity levels, wind speed, and rainfall can be confounding factors18. The association between short-term air quality and schizophrenia outpatient visits with various lag days was investigated using a time series Poisson regression model. Concentrations of PM10, SO2, and NO2, as well as the daily mean humidity levels and average temperature, allow modifying the possible impact of weather on hospital admissions27.
E (Yβ) represents the reported daily number of hospital admissions on day t, as well as the coefficients between pollutants and hospital admissions respectively, ns is a date-time natural cubic spline function; St is the daily average of air pollutants on day t; D means the day of the week; 3 is degrees of freedom (df) used for time and humidity (H); 6 is df used for average temperature (T) and b is the intercept. When this core model is created, it is used by inserting air pollution concentrations into a single-pollutant model, researchers can look into the link between schizophrenia admissions and air pollution. Several lag patterns were incorporated as sensitivity tests in the core models since health effects might last for several days. Single-day delays and moving average lags (lag 1 to lag 3) can be used to assess the delayed consequences of pollutants. Two-pollutant models can be considered for examining the stability of effects after adjusting for co-pollutants.
Data sources and software tools of the study
Time series environmental data can be obtained across a wide variety of resources; from mobile phone sensors to more sophisticated monitoring tools and databases operated by state, federal agencies, and organizations. Many researchers examined data sets from online outlets, such as Kaggle. The temperature variables can be collected from the respective country's Bureau of Meteorology, including relative humidity, rainfall, atmospheric pressure, and wind directions. Satellite data may be available to measure green space. A data collection from the Landsat program for Denmark is available28. The authors used Danish national registers providing information on all people living in Denmark to examine traffic-related exposures that influence schizophrenia risk29,30. Standard Model Instrumentation for Noise Assessments (STAMINA) can be used for estimating residential traffic noise levels31. In India, pollution data can be collected from the Central Pollution Control Board (CPCB). All major air pollutants and noise quality data are freely available on official websites. India Meteorological Department (https://mausam.imd.gov.in) will provide all kinds of climate data for researchers. The Automated Meteorological Data Acquisition System of Japan can collect weather data from meteorological satellites containing altitude, location, and temporal information32.
The major source of psychiatric data in this research is emergency admission statistics from hospitals33. Another important source is patient data from insurance companies. Some studies analyzed daily data of outpatient admissions. The data from a teenage national well-being study in the Netherlands, including psychiatric trauma questions focused on the Kessler 10 scale31. In quantifying psychiatric illness, parent assessment tools and sub-scale scores of anxiety, depressive symptoms, somatic symptoms, and withdrawal scales using the behavior assessment system for children (BASC) are suitable19. Symptom-Checklist-90-Revised Scale (SCL-90-R) can be considered for life transition stress and cognitive stress assessment34. The National Morbidity, Mortality, and Air Pollution Study (NMMAPS) data set is accessible to the public via the Internet-based Health and Air Pollution Surveillance System website. It contains 5114 observations of daily mortality as well as meteorological and pollution information for Chicago.
The DLNM kit inside the R statistical environment includes a range of tools to define and analyze the effects of lag. This structure is introduced in the 'DLNM' R bundle, which offers functions to execute a wide variety of models within the DLNM family, with a focus on graphs, and emphasis on graphical representation2. Most statistical studies of the problem mentioned were carried out using R tools with the following packages (version 4.1.3): 'mgcv', 'nlme', data.table, Hmisc, landsat, lubridate, plyr, raster rgdal, RStoolbox, sp28,35,36. Statistical analysis can be done by Stata17, WEKA version 3.9.6, and SAS version 9.4 software23,24 .
Classification based on techniques and input variables
.PNG)
Figure 2: Techniques used in finding the impact of environment on mental health
.PNG)
Figure 2: Techniques used in finding the impact of environment on mental health
The major applied techniques
Based on the literature review, it was found that very few data analysis techniques have been tested on the specified problem. Most of the studies used statistical techniques to explain the exposure-response relationship between environment and mental health37. Any of these components or a combination of one or more components make data mining a reality. All related studies are either descriptive or explanative to identify seasonal variation and also to understand cause and effect. Some exploratory analysis highlights time series data in a visual format. The utility of competing methods varies based on the nature of the response variable, the sample size, the number of involved exposure variables, and the frequency of the exposure-response association. The papers were classified into different clusters based on the techniques used. Major techniques applied in finding the impact of the environment on mental health are shown in Figure 2.
Regression methods: Regression methods provide the means to achieve accurate estimates of performance variables dependent on a group of predictors. Methods of regression are divided into four classes including a selection of variables, latent variables, methods of penalized regression, and ensemble methods. For the model making, a subset of predictors is selected, and the others are set aside. The ultimate model has a similar pattern to multiple linear regression (MLR),
yˆ = Xb+ ε 38 (Eq. 6)
In which, the predicted answer is yˆ, X is the expanded regressor matrix, a column for the intercept and b is the regression coefficients obtained by minimizing the number of residual squares, ε38. The variables used and results of papers implemented regression techniques are summarized in Table 1.
Based on the literature review, it was found that very few data analysis techniques have been tested on the specified problem. Most of the studies used statistical techniques to explain the exposure-response relationship between environment and mental health37. Any of these components or a combination of one or more components make data mining a reality. All related studies are either descriptive or explanative to identify seasonal variation and also to understand cause and effect. Some exploratory analysis highlights time series data in a visual format. The utility of competing methods varies based on the nature of the response variable, the sample size, the number of involved exposure variables, and the frequency of the exposure-response association. The papers were classified into different clusters based on the techniques used. Major techniques applied in finding the impact of the environment on mental health are shown in Figure 2.
Regression methods: Regression methods provide the means to achieve accurate estimates of performance variables dependent on a group of predictors. Methods of regression are divided into four classes including a selection of variables, latent variables, methods of penalized regression, and ensemble methods. For the model making, a subset of predictors is selected, and the others are set aside. The ultimate model has a similar pattern to multiple linear regression (MLR),
yˆ = Xb+ ε 38 (Eq. 6)
In which, the predicted answer is yˆ, X is the expanded regressor matrix, a column for the intercept and b is the regression coefficients obtained by minimizing the number of residual squares, ε38. The variables used and results of papers implemented regression techniques are summarized in Table 1.
Table 1: Summary table of papers that used different regression methods
The relationship between particulate matter (PM) and the severity of mental health have been investigated in many papers using a wide range of regression techniques or its combination. Major classifications are logistic regression and linear regression. Time-series Poisson regression model is most common in these types of studies. Eguchi39 used multivariate logistic regression and determined that ambient PM2.5 concentration was associated with the exacerbation of schizophrenia. Pedersen et al. found that geographical distance from residence to the nearest major road had a significant effect on schizophrenia. The highest risk was found in children living 500–1000 meters from the nearest major road42. Liang27 found that short-term air pollutants, such as PM10, SO2, and NO2 exposure might contribute to the increased risk of outpatient visits for schizophrenia. Even though there is no universal supremacy of one technique, regression techniques have been widely used for this problem. There was a finding that hospital admissions increased with increasing levels of PM2.5 during the summer, which was analyzed using Poisson regression techniques43. The relationships between the PM and the hospital admission for schizophrenia were assessed using a time-series Poisson regression model with the duration of hospital admission as the relevant variable41. In several lag models, the strongest correlations were seen on the sixth day. Increased likelihood of hospital admissions for schizophrenia was linked to PM air pollution, with greater relationships among married and female patients. This result is not in line with other researchers' findings.
Correlations: In psychological science, the Pearson correlation coefficient and the Spearman rank correlation coefficient are commonly used. Using models of low to high sample sizes, for normally distributed data, both have similar predicted values, but Spearman rank correlation is more variable, especially when the correlation is strong44. The papers that implemented Pearson and Spearman correlation techniques are summarized in Table 2. Pearson and Spearman correlation was used to find the impact of pollution on admission rates of schizophrenia patients44. One of the studies was related to air pollutant concentrations and data on respiratory disease inpatients in urban area8. Referring to such papers will give an insight into applying this technique to any type of psychiatric disorder. The studies by Shiloh et al. 45 Yackerson et al. 46 were conducted on the role of solid air-suspended particle (SSP) concentration in the occurrence of mental disorders. A significant correlation was found between variations of SSP number concentration and number of suicide attempts. Shiloh et al. used monthly hospital admissions and annual admissions of schizophrenia to find weather influences45. They found that schizophrenia patient’s mean monthly admission rates correlated with the mean maximal monthly environmental temperature.
Lag-based models: A modelling paradigm to flexibly explain correlations demonstrating the time series data with potentially non-linear and delayed effects is DLNMs. A modelling approach that may concurrently reflect delayed effects and non-linear exposure-response relationships is the class of DLNM. It is based on the definition of a cross-basis, a bi-dimensional space of functions that together describe the form of connection along the range of the predictor and the lag dimension. Distributed lag models (DLMs) have elegantly defined delayed effects; a technique used in research on environmental factors to measure health effects2.
The dependent (Y) variable is an observable count that fits the Poisson distribution and is analogous to periodic multiple regression. Therefore, non-negative integers are the potential values of Y: 0, 1, 2, 3, and so on. The Poisson distribution predicts the probabilities of events (i.e. loss, death, or existence). Experiments investigating the short-term consequences of stressors from the climate have recently raised the question of delayed impacts. The papers plotted the lag effect using Poisson Regression and DLNM techniques summarized in Table 3. Major limitations and future directions of the Poisson and DLNM cluster are pointed out in discussions. The question of "Is air quality linked to increased schizophrenia admissions?" was addressed by Duan et al. 15, Liang et al. 27, and Pedersen et al. 42 using this lag model. The findings indicated that short-term air pollutant exposure has a statistically significant effect on schizophrenia admissions. The pollution generated from road traffic may have a significant effect on schizophrenia admissions30,47. The geographical distance from the residence to the nearest major road had a significant lagged effect42. Another DLNM output with the strongest effect occurring at a two-day lag was high humidex (humidity index) which was substantially related to the development of schizophrenia and the more susceptible patients were in the 21-60 years age group, male patients, and married patients48.
Other techniques: To test the relationship between meteorological factors and suicide, an apriori algorithm was used for their association2. The apriori algorithm was used to derive migraine-related feelings and explore the possible correlations between migraine symptoms and temperature influences3.
Lag-based models: A modelling paradigm to flexibly explain correlations demonstrating the time series data with potentially non-linear and delayed effects is DLNMs. A modelling approach that may concurrently reflect delayed effects and non-linear exposure-response relationships is the class of DLNM. It is based on the definition of a cross-basis, a bi-dimensional space of functions that together describe the form of connection along the range of the predictor and the lag dimension. Distributed lag models (DLMs) have elegantly defined delayed effects; a technique used in research on environmental factors to measure health effects2.
The dependent (Y) variable is an observable count that fits the Poisson distribution and is analogous to periodic multiple regression. Therefore, non-negative integers are the potential values of Y: 0, 1, 2, 3, and so on. The Poisson distribution predicts the probabilities of events (i.e. loss, death, or existence). Experiments investigating the short-term consequences of stressors from the climate have recently raised the question of delayed impacts. The papers plotted the lag effect using Poisson Regression and DLNM techniques summarized in Table 3. Major limitations and future directions of the Poisson and DLNM cluster are pointed out in discussions. The question of "Is air quality linked to increased schizophrenia admissions?" was addressed by Duan et al. 15, Liang et al. 27, and Pedersen et al. 42 using this lag model. The findings indicated that short-term air pollutant exposure has a statistically significant effect on schizophrenia admissions. The pollution generated from road traffic may have a significant effect on schizophrenia admissions30,47. The geographical distance from the residence to the nearest major road had a significant lagged effect42. Another DLNM output with the strongest effect occurring at a two-day lag was high humidex (humidity index) which was substantially related to the development of schizophrenia and the more susceptible patients were in the 21-60 years age group, male patients, and married patients48.
Other techniques: To test the relationship between meteorological factors and suicide, an apriori algorithm was used for their association2. The apriori algorithm was used to derive migraine-related feelings and explore the possible correlations between migraine symptoms and temperature influences3.
Table 2: Summary of papers using Pearson and Spearman correlations

To analyze mental illness and environmental factors, apriori algorithm is rarely used. Given that the data analysis techniques are not limited to the above-mentioned methods, depending on the problem and type of data sets, a researcher may get more choices. For example, an analysis of the correlation between sub-group characteristics like age, gender, marital status, and employment status, may need algorithms of deep neural networks49.
Based on climate variables
Climate variables influence mental well-being50. The major climate factors investigated were temperature and sunlight. Humidity, rainfall, wind intensity, and atmospheric pressure were major cofounders. Some important findings of previous studies are presented in Table 3.
Climate variables influence mental well-being50. The major climate factors investigated were temperature and sunlight. Humidity, rainfall, wind intensity, and atmospheric pressure were major cofounders. Some important findings of previous studies are presented in Table 3.
Table 3: Summary of lag effect of environmental impact on schizophrenia
| Author(Ref) | Problem Addressed | Climate/ Pollution variables | Disease and patient variables | Lag effect |
| De-sheng Zhao et al.48 | Daly temperature and schizophrenia emergency admissions | DTR, Confounders, such as temperatures, relative humidity, seasonal patterns and long-term, weekday and holiday averages. | Age, gender and marital status, the predicted number of schizophrenia cases on any given day. | The adverse effects of extremely high-temperature variations occurred immediately and decreased to lag 6 days. |
| Duan J et al.15 | Air quality with schizophrenia admissions | NO2, PM10, and SO2 had a five-day, four-day, and ten-day delayed effect. | Based on gender, age groups and occupation. | The risk effects of pollutants occurred to lag 0–1 to lag 0–5 for NO2 and PM10, lag 0–2 to lag 0–10 for SO2. |
| Pan R et.al51 | The effect of heat and cold on schizophrenia hospitalizations | Daily highest temperature, lowest temperature, humidity levels, wind speed, sunshine per hour | Subgroup analysis of age, gender and marital status. | The effect of temperature on hospitalizations is mainly attributed to heat exposure. The lag effect is not explored. |
| Gu S et.al52 | Sunlight exposure and schizophrenia inpatient admissions | Temperature, relative humidity, rainfall and sunshine duration | Admission date, sex, age, and address of the patient, diagnosis and ICD-10 codes | The effect of sunshine duration with a lag of 0 to 21 days is visible. |
| Liang Z et.al27 | Short-term air quality exposure and hospital appointments of schizophrenia. | The hourly data - the total emission rate of air pollutants. Average regular relative humidity and mean temperature | Outpatient visits characteristics such as residence, age, and gender. | The significant association of PM10 is within the same days and for NO2 at lag 1. For SO2 lag associations is more significant in all the single lag models. |
| Wang et.al18 | Temperature and schizophrenia patient admissions | Temperature variations, relative humidity, wind intensity, and rainfall | Daily hospital data on age, gender, marital status, onset season, and place of living. | The greatest effect of temperature on schizophrenia onset was observed on days 1, 2, and 3 with a 3-day lag. |
| Pedersen et.al42 | Urban birth raises and traffic related exposure to schizophrenia. | Degree of urbanization. Geographical distance from the home to the closest main road is determined. |
Data on hospital admissions. Parents and siblings with a diagnosis of schizophrenia | No evidence that the distance to the nearest major road had an impact on schizophrenia. Traffic-related exposures may have less impact on urban-rural differences. |
Impact of temperature: The relationship between temperature and schizophrenia has been widely studied, albeit with conflicting findings. The assumption of satisfaction with the temperature result has been linked to schizophrenia diagnosis 18,25,45. The relative risks (RR) for exceedingly high DTR change were shown to be significantly associated with greater schizophrenia hospitalizations, while no such associations were seen for relatively higher DTR change26. The adverse effect of the average temperature on schizophrenia onset showed the lag effect of 1, 2, and 3 days after the onset, with the greatest risk factor at the 3-day lag. Men were more likely than women to be hospitalized for schizophrenia25. Individuals aged 15–29 and 50–64 years were exposed to high levels of DTR, and they were shown to be more susceptible to the onset of schizophrenia. Male patients were more likely than female patients to have a link between high DTR and schizophrenic onset. Also, male patients aged 21-60, as well as married patients were more sensitive to high temperatures, with heat effects occurring with 1-day lag18. According to studies, DTR had a greater impact on married patients with schizophrenia than on single patients with schizophrenia26. It was proven that high temperatures had a delayed reaction in schizophrenia hospitalizations. A temperature of 28 0C with a 0-4-day lag was associated with an increase of 7% in admissions18.
Impact of other climate variables: One of the frequently used climate variables is sunlight. Gu et al. 52, in a study conducted in Ningbo, China, reported a relationship between lack of exposure to sunlight and increased risk of hospital admissions for schizophrenia. Another variable in consideration was humidity levels53, which has been used as an environmental covariate in many studies18,45,52. De-sheng et al. found an impact of humidex on schizophrenia48. They found that patients aged 21-60, males, and married patients were most susceptible to the effects of high humidex, which was a risk factor for the onset of schizophrenia. No study was found revealing the effect of humidity on schizophrenia. Air pressure, precipitation, and cloudiness were used as possible confounding factors in the study of the effect of air-suspended particulate on the incidence of schizophrenia44. There was no significant correlation between these covariates. All climate variables were considered covariates in pollution-based studies. Body discomfort index45, wind speed18,51, and rainfall18 were also not found as potential cofounders in the analysis of the problem.
Pollution
Pollution is generally classified in terms of air, noise, and water. There are a wide range of air pollutants because of carbon emission and highly populated lifestyle of cities. Traffic congestion noise may be linked to increased levels of noise annoyance, which may create isolation and loneliness, and interpersonal separation in the area, which result in mental illness40. There was no research investigating the relationship between water pollution and schizophrenia. The present review mentions the impact of air pollution and noise pollution according to various studies. PM2.5, PM10, NO2 SO2, SSP, CARBON, NDVI (a measure of green space), and indoor and outdoor noise quality were various pollution parameters used in the studies.
Impact of air pollution: The surface ambient layer contains both neutral or charged gas contaminants and SSP. PM10, SO2, and NO2 are the primary air contaminants. A major problem in air quality-based research is that pollutant concentrations are constant phenomena in the atmosphere, but their observations are normally available at a small number of sampling stations or are derived from computational models. Many studies have revealed that air quality is associated with mental health problems31. Some findings revealed a connection between certain PM and various schizophrenia forms54. According to Liang27, the positive relation of NO2 remained considerable in lag 1. The delayed correlations of SO2 were significantly more evident than those of NO2 and PM10, and they remained significant in lag 1 to lag 3 in single lag models. NO2 and PM10 had 4-day and 3-day narrow impacts, respectively. For ten days, SO2 had a stronger effect. The RRs for high NO2 concentrations were shown to be significantly associated to an increase in schizophrenia patients.
Duan et al. concluded that pollution effects include lag 1 to lag 3 for Nitrogen dioxide and PM10, and lag 2 to lag 9 for Sulphur dioxide in single-day lag structures15. For a two-day lag period, the effect of PM2.5 concentration was substantial39. Urbanization and teenage psychotic episodes are associated with NO2 and Nox23. The relationship between PM2.5 levels and age increased considerably in patients aged over 65 years, according to Liang et al. 27. Although still not statistically relevant, the associations between environmental pollution and schizophrenia seemed to be higher in females than males in sex-based models. The findings of Liu et al. indicated that children are more vulnerable to the concentration of PM2.535.
Impact of noise pollution: The higher annoyance of residential noise (LAeq) is associated with higher sleep disturbance and mental ill-health. Few existing studies have found correlations between noise and hearing problems, including mental well-being and cognitive development, as well as non-auditory health conditions. Noise from trains was found to be linked to psychological discomfort55. In multi-exposure studies, correlations with nearby greenery and air pollution were studied but were less significant. Environmental noise stress has a deleterious impact on attention, cognitive function, and episodic memory, among other brain functions56. Noise pollution in cities may cause chronic stress levels and impede the growth of typically developing brains and behaviors 57. According to Dutch population-based studies, urban regions tend to have a higher prevalence of stressful conditions like crime, relationship breakdown, noise pollution, a sense of unease, and poor mental and physical health58. Children may be more sensitive to noise impacts because they may have the less cognitive capacity to grasp ecological challenges and anticipate stressors, and may require effective measures of adaptation to noise control57.
Other forms of pollution: In the present review, any article addressing the impact of water pollution or other forms of pollution on schizophrenia was not found. Unlike air pollution or noise pollution which have an effect in measuring water pollution and analysis, its impact on schizophrenia is not easily doable. There is no clear-cut idea of the source of water that is individually consumed. That is also variations in water source depending on region/city. Some places have pipe water supply and this could be compared with hospital division data. However, for a city like Bangalore or any other city in the developing world, the residents may resort to multiple sources of water like wells, pump storage, or ponds. The researchers were not able to find any technical article that could relate to water pollution and schizophrenia admissions. Similarly, for other forms of pollution, no studies were found that correlates those forms of pollution and schizophrenia admission.
Other factors
Some articles investigated the impact of urbanization and other environmental facets, including noise and traffic42,57. The results agree with the suggestion by lewis et al.59 that environmental factors found in cities increase the risk of schizophrenia. Green area exposure is a unique environmental risk factor for the development of schizophrenia. The mechanism behind this association is uncertain, although exposure to more green space throughout childhood has been linked to a lower incidence of schizophrenia28. Green space was found to be inversely related to mental health issues in single-exposure analyses. A study on green space calculated from normalized difference vegetation index (NDVI) is another major attribute28,31. The processes underlying this beneficial impact of green space concerning schizophrenia have to be answered by critical new research questions.
Results
Preliminary analysis of Bangalore data
Bangalore is a metropolitan city despite being in a tropical region of India. To test the feasibility of existing studies in Indian cities, they were replicated using data from Bangalore city. A new investigation of the problem was not the target of this paper. To test the scope and applicability of existing studies in Bangalore, daily concentrations of PM2.5, PM10, CO, and temperature were considered. First, the correlation between these variables and schizophrenia admissions was checked using the Spearman correlation. The normality of data was checked with the Shapiro-Wilk normality test, which was non-normal. Patient admission data was collected from hospitals located in Bangalore. Patients’ data between 2017 November to 2021 January were collected, which may be severe schizophrenia cases. The data were purely filtered for schizophrenia or schizoaffective patients which may only be 30% of total psychiatric patients reporting in Bangalore hospitals. Pollutants were collected from the central pollution control board of India. The mean values of 3 major zones of the city were considered for the correlation analysis.
In the primary feasibility study, PM2.5, PM10, and the temperature had a positive correlation with the daily number of emergency admissions of schizophrenia. Figure 3 illustrates Spearman correlations between environmental variables and the number of admissions (NoA) of schizophrenia. CO did not have any lag effect on NoA in Bangalore city. City temperature was positively correlated with NoA and statistically significant in the spearman test (p = 0.05, confidence interval = 95%). This positive correlation was the motivation to explore more Bangalore data and then the lag effect of these environment variables was studied on schizophrenia. The existing techniques were applied to evaluate whether Bangalore data is also suitable for establishing a relationship between the mentioned variables and schizophrenia.
Impact of other climate variables: One of the frequently used climate variables is sunlight. Gu et al. 52, in a study conducted in Ningbo, China, reported a relationship between lack of exposure to sunlight and increased risk of hospital admissions for schizophrenia. Another variable in consideration was humidity levels53, which has been used as an environmental covariate in many studies18,45,52. De-sheng et al. found an impact of humidex on schizophrenia48. They found that patients aged 21-60, males, and married patients were most susceptible to the effects of high humidex, which was a risk factor for the onset of schizophrenia. No study was found revealing the effect of humidity on schizophrenia. Air pressure, precipitation, and cloudiness were used as possible confounding factors in the study of the effect of air-suspended particulate on the incidence of schizophrenia44. There was no significant correlation between these covariates. All climate variables were considered covariates in pollution-based studies. Body discomfort index45, wind speed18,51, and rainfall18 were also not found as potential cofounders in the analysis of the problem.
Pollution
Pollution is generally classified in terms of air, noise, and water. There are a wide range of air pollutants because of carbon emission and highly populated lifestyle of cities. Traffic congestion noise may be linked to increased levels of noise annoyance, which may create isolation and loneliness, and interpersonal separation in the area, which result in mental illness40. There was no research investigating the relationship between water pollution and schizophrenia. The present review mentions the impact of air pollution and noise pollution according to various studies. PM2.5, PM10, NO2 SO2, SSP, CARBON, NDVI (a measure of green space), and indoor and outdoor noise quality were various pollution parameters used in the studies.
Impact of air pollution: The surface ambient layer contains both neutral or charged gas contaminants and SSP. PM10, SO2, and NO2 are the primary air contaminants. A major problem in air quality-based research is that pollutant concentrations are constant phenomena in the atmosphere, but their observations are normally available at a small number of sampling stations or are derived from computational models. Many studies have revealed that air quality is associated with mental health problems31. Some findings revealed a connection between certain PM and various schizophrenia forms54. According to Liang27, the positive relation of NO2 remained considerable in lag 1. The delayed correlations of SO2 were significantly more evident than those of NO2 and PM10, and they remained significant in lag 1 to lag 3 in single lag models. NO2 and PM10 had 4-day and 3-day narrow impacts, respectively. For ten days, SO2 had a stronger effect. The RRs for high NO2 concentrations were shown to be significantly associated to an increase in schizophrenia patients.
Duan et al. concluded that pollution effects include lag 1 to lag 3 for Nitrogen dioxide and PM10, and lag 2 to lag 9 for Sulphur dioxide in single-day lag structures15. For a two-day lag period, the effect of PM2.5 concentration was substantial39. Urbanization and teenage psychotic episodes are associated with NO2 and Nox23. The relationship between PM2.5 levels and age increased considerably in patients aged over 65 years, according to Liang et al. 27. Although still not statistically relevant, the associations between environmental pollution and schizophrenia seemed to be higher in females than males in sex-based models. The findings of Liu et al. indicated that children are more vulnerable to the concentration of PM2.535.
Impact of noise pollution: The higher annoyance of residential noise (LAeq) is associated with higher sleep disturbance and mental ill-health. Few existing studies have found correlations between noise and hearing problems, including mental well-being and cognitive development, as well as non-auditory health conditions. Noise from trains was found to be linked to psychological discomfort55. In multi-exposure studies, correlations with nearby greenery and air pollution were studied but were less significant. Environmental noise stress has a deleterious impact on attention, cognitive function, and episodic memory, among other brain functions56. Noise pollution in cities may cause chronic stress levels and impede the growth of typically developing brains and behaviors 57. According to Dutch population-based studies, urban regions tend to have a higher prevalence of stressful conditions like crime, relationship breakdown, noise pollution, a sense of unease, and poor mental and physical health58. Children may be more sensitive to noise impacts because they may have the less cognitive capacity to grasp ecological challenges and anticipate stressors, and may require effective measures of adaptation to noise control57.
Other forms of pollution: In the present review, any article addressing the impact of water pollution or other forms of pollution on schizophrenia was not found. Unlike air pollution or noise pollution which have an effect in measuring water pollution and analysis, its impact on schizophrenia is not easily doable. There is no clear-cut idea of the source of water that is individually consumed. That is also variations in water source depending on region/city. Some places have pipe water supply and this could be compared with hospital division data. However, for a city like Bangalore or any other city in the developing world, the residents may resort to multiple sources of water like wells, pump storage, or ponds. The researchers were not able to find any technical article that could relate to water pollution and schizophrenia admissions. Similarly, for other forms of pollution, no studies were found that correlates those forms of pollution and schizophrenia admission.
Other factors
Some articles investigated the impact of urbanization and other environmental facets, including noise and traffic42,57. The results agree with the suggestion by lewis et al.59 that environmental factors found in cities increase the risk of schizophrenia. Green area exposure is a unique environmental risk factor for the development of schizophrenia. The mechanism behind this association is uncertain, although exposure to more green space throughout childhood has been linked to a lower incidence of schizophrenia28. Green space was found to be inversely related to mental health issues in single-exposure analyses. A study on green space calculated from normalized difference vegetation index (NDVI) is another major attribute28,31. The processes underlying this beneficial impact of green space concerning schizophrenia have to be answered by critical new research questions.
Results
Preliminary analysis of Bangalore data
Bangalore is a metropolitan city despite being in a tropical region of India. To test the feasibility of existing studies in Indian cities, they were replicated using data from Bangalore city. A new investigation of the problem was not the target of this paper. To test the scope and applicability of existing studies in Bangalore, daily concentrations of PM2.5, PM10, CO, and temperature were considered. First, the correlation between these variables and schizophrenia admissions was checked using the Spearman correlation. The normality of data was checked with the Shapiro-Wilk normality test, which was non-normal. Patient admission data was collected from hospitals located in Bangalore. Patients’ data between 2017 November to 2021 January were collected, which may be severe schizophrenia cases. The data were purely filtered for schizophrenia or schizoaffective patients which may only be 30% of total psychiatric patients reporting in Bangalore hospitals. Pollutants were collected from the central pollution control board of India. The mean values of 3 major zones of the city were considered for the correlation analysis.
In the primary feasibility study, PM2.5, PM10, and the temperature had a positive correlation with the daily number of emergency admissions of schizophrenia. Figure 3 illustrates Spearman correlations between environmental variables and the number of admissions (NoA) of schizophrenia. CO did not have any lag effect on NoA in Bangalore city. City temperature was positively correlated with NoA and statistically significant in the spearman test (p = 0.05, confidence interval = 95%). This positive correlation was the motivation to explore more Bangalore data and then the lag effect of these environment variables was studied on schizophrenia. The existing techniques were applied to evaluate whether Bangalore data is also suitable for establishing a relationship between the mentioned variables and schizophrenia.
.PNG)
Figure 3: Correlation of PM2.5, PM10, Temp, and CO with NoA in Bangalore city
In the hospitals of Bangalore city, data collection that is also in digital form is rare and tough. The patient data from psychiatric hospitals were recorded in paper files. The sample data collected from hospitals located in various parts of the city may represent the schizophrenia population of the whole city. Three peaks of schizophrenia cases were observed in Bangalore city in January 2018, January 2020 and December 2020. Visualization of expected impacts along with contaminants for particular delays is shown in a contour plot (Figure 4). It shows the lag-specific association between these variables and schizophrenia cases. In general, positive associations were found that are non-linear lag (in days) patterns between PM2.5, PM10, temperature, and NoA, but none for CO. The estimated RR value for moderate levels of PM2.5 with a lag of 5 days was 2.7. RR for PM10 and temperature with the same lag was 1.7 and 1.3, respectively. In the case of CO, the RR was zero. The overall RR for low levels of PM2.5 and temperature without lag effect were 1 and 1.2, respectively. There was no risk found for lower values of PM2.5. Lag effects were studied with 99% confidence intervals. With a powerful immediate effect and delayed effect of pollution, these plots reveal various patterns for the effect of low and high pollutant concentrations.
.PNG)
Figure 4: Lag-specific effects with NoA in terms of RR
Ethical issues
This review reports studies involving daily hospital admission count and freely available pollutant data. The data affecting human privacy were not included. The data were analyzed using open-source software.
Discussion
Research issues
Many researchers have used hospital admission data in their studies. Prescription details provided by the insurance company have been used in some studies 31. The assumption made here is that the data recorded is accurate. However, there may be errors while recording the data at any level. The data recorded digitally may only relate to patients who are admitted. This may not include details of patients who had consulted a doctor but did not seek admission. Another assumption made was that the patient was a local resident and had endured the climatic and pollution factors as recorded. A patient might have traveled from a different place, and the lag effect could have been felt in the new place. Exposure misrepresentation exists as a potential weakness. Many factors, like participants who spent a significant amount of time indoors or away from their specified residence, may affect the recorded data for hospital admissions27,52. Dzhambov et al.55 did not collect indoor noise exposure (e.g., from neighbors) when individuals spend less time outdoors than in summer. A more precise emissions exposure calculation can be accomplished by considering other areas where patients spend a large proportion of their time. More research is required to investigate the relationship between children's exposure to air pollution and psychotic symptoms and other psychological conditions23. Most of the studies did not consider indoor fuel and wood combustion for domestic energy which may not be possible in hospital-based studies.
The relationship between atmospheric temperature and schizophrenia18 can be affected by uncertain factors such as educational age, family history, drug usage, air contaminants, and lack of comprehensive data on first admissions or re-admissions. During summer when patients stay indoors, the effects of the external factors may not get recorded54. The use of air filters indoors or the use of room heaters during winter might alter the climatic parameters within a confined space. Any observed hospital admission or lack of it may be due to extraneous factors. Thus, there might be issues with the data recorded, which is another challenge for this problem. There was a lack of training data on cases of AQI values greater than 300 in the approach to determining health risks dependent on air quality standards60.
There have been other articles with contradictory findings, for instance, a study from Canada claimed that higher temperatures were associated with an increase in the prevalence of schizophrenia61. Many researchers have looked at the association between temperature and schizophrenia in various regions, and a rise in the frequency of schizophrenia-related emergency hospital visits has been documented as a result of daily temperature shift13,62,63, suggesting the existence of a delayed effect26,64. A thorough study of the prevalence of schizophrenia by Saha et al.65 revealed an increasing trend for schizophrenia by increasing latitude, indicating that regional differences may exist in the impacts of temperature 10,66. However, a study in Taiwan's tropical environment discovered a relationship between air temperature and hospitalizations for schizophrenia, revealing that cold weather may be a risk factor for the development of schizophrenia67. Due to the lack of sufficient research in India, it is suggested to explore this association in future studies. In the majority of the studies15,18,26, data was gathered from one region which may not be generally applicable. The results may not valid for other countries/regions. The time series data of schizophrenia was generally small. A relatively small sample size was used in many studies51. Specific age ranges (like 20 to 59 years) demonstrated greater vulnerability to the emergence of schizophrenia that may be caused by the development of schizophrenia at a young age or a small sample size, further research is required in such cases15. Data fusion in smart city environments is also a difficult consideration in the collection and analysis of data from disparate data sources68. The biological mechanism/reason behind the mysterious relationship between pollution and schizophrenia needs to be investigated further, which is not the intention of this review study.
Scope for further research
External validity can be improved by including different cities. There is also a need for research that spans multiple cities. The biological reason behind the exposure-response relation is also a matter of further research. The variables suggested are the length of the illness, treatment status, smoking or other forms of tobacco consumption, academic history, profession, and birthplace. Individual living environments and situations are not difficult to consider. SSP in the occurrence of mental disorders46 has been less investigated. Hospital outpatient visits characteristics, such as location, age, gender, and number of schizophrenia cases on the day, are the major attributes considered for the association. Subgroup analyses of age, gender, and marital status are also common in the literature. In the study of traffic-related exposure to air pollution and symptoms of psychiatric disorders especially in children19, underlying genetic vulnerability also can be considered in the future. The findings 42 of Pedersen et al. on traffic-related exposures, which were not responsible for the urban-rural disparities in schizophrenia risk, need replication. Time series studies with at least 3 years of weather data are required51 in some studies. Sample distribution and more health impairments for review should be included. Potential confounders, including BMI, level of education, cigarette behaviors, and medical histories were not available in many of the investigations, which might have influenced the correlations between air pollutants and schizophrenia. Collection of this kind of co-founders is also a difficult task because of the non-availability of such data in digital form and the privacy of individuals. The lack of indications of the severity of the condition, such as repeated hospital admissions, may restrict the in-depth examination of contaminants' involvement. Future studies require the application of simulated modelling scenarios to test the health impacts of environmental change and to validate whether the same model may be used to forecast psychiatric admissions from air pollution69.
Although some authors considered other data mining techniques, such as time series association rules70, different statistical, and machine learning techniques71, these techniques have not gained popularity as much as regression, DLNM, and correlation techniques on this problem. Across all situations and all parameters, there is no universal superiority by one system. The output varies according to the nature of the response component, the sample size, the number of contaminants involved, and the frequency of the association/interaction between exposure and response. Neural networks can be used in future research to explore the biological mechanism behind this association and also to reveal more underlying relationships between pollution and schizophrenia49,72,73.
Conclusion
In this review study, the impact of pollution and climate on schizophrenia was explored as available from existing literature. Dependencies between factors that predict pollutant intensity and clinical outcomes were predicted by the researchers. DLNM-based models are leading in exploring this association. The majority of them were mainly from Chinese cities to study the lag effect of pollutants on schizophrenia. It was found that different weather variables especially temperature may contribute to the development of psychosis in schizophrenia patients, potentially raising their admission rates to psychiatric facilities. The pollutants like PM, NO2, and SO2 also had a lag effect on schizophrenia. Some age and sex groups displayed greater susceptibility than other groups to schizophrenia emergence, which may be affected by schizophrenia onset or limited sample size. It is important to look into the basic biological mechanisms that underpin the relationship between environmental variables and schizophrenia admissions. Time series association techniques and deep learning algorithms have not experimented on this problem. These techniques may reveal unexplored aspects of the exposure-response problem. Temperature and major pollutants were explored more and noise pollution-based studies are comparatively less on schizophrenia. Additional research into several cities in different countries is required to improve the external validity of the study, including individual living environments and situations. The majority of findings need replication to validate their findings in different regions and conditions. The primary analysis of Bangalore data found that the association between environmental variables and schizophrenia is completely valid for detailed research in Indian cities. Urban-rural differences in the mental health domain are another interesting area for further study.
In this paper, we evaluated Bangalore data and found that the relationships mentioned for Chinese cities are also applicable to Indian data. Thereby, the researchers ascertained the environmental-schizophrenia relationships applicable across the globe. In the process, a rudimentary DLNM model was applied to determine the lag effect of environmental variables on schizophrenia. The primary results could be improved by exploring better models and algorithms as part of future work.
Acknowledgment
Thanks are owed to the hospitalization data provided by Bangalore hospitals including Cadabam hospitals, People Tree Maarga hospital, and Spandana hospital, as well as central pollution control board (CPCB) of India for providing data access through website.
Funding
The author(s) received no financial support for the research or publication of this review.
Conflict of interest
The authors declare that there is no conflict interest.
This is an Open-Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt, and build upon this work for commercial use.
References
This review reports studies involving daily hospital admission count and freely available pollutant data. The data affecting human privacy were not included. The data were analyzed using open-source software.
Discussion
Research issues
Many researchers have used hospital admission data in their studies. Prescription details provided by the insurance company have been used in some studies 31. The assumption made here is that the data recorded is accurate. However, there may be errors while recording the data at any level. The data recorded digitally may only relate to patients who are admitted. This may not include details of patients who had consulted a doctor but did not seek admission. Another assumption made was that the patient was a local resident and had endured the climatic and pollution factors as recorded. A patient might have traveled from a different place, and the lag effect could have been felt in the new place. Exposure misrepresentation exists as a potential weakness. Many factors, like participants who spent a significant amount of time indoors or away from their specified residence, may affect the recorded data for hospital admissions27,52. Dzhambov et al.55 did not collect indoor noise exposure (e.g., from neighbors) when individuals spend less time outdoors than in summer. A more precise emissions exposure calculation can be accomplished by considering other areas where patients spend a large proportion of their time. More research is required to investigate the relationship between children's exposure to air pollution and psychotic symptoms and other psychological conditions23. Most of the studies did not consider indoor fuel and wood combustion for domestic energy which may not be possible in hospital-based studies.
The relationship between atmospheric temperature and schizophrenia18 can be affected by uncertain factors such as educational age, family history, drug usage, air contaminants, and lack of comprehensive data on first admissions or re-admissions. During summer when patients stay indoors, the effects of the external factors may not get recorded54. The use of air filters indoors or the use of room heaters during winter might alter the climatic parameters within a confined space. Any observed hospital admission or lack of it may be due to extraneous factors. Thus, there might be issues with the data recorded, which is another challenge for this problem. There was a lack of training data on cases of AQI values greater than 300 in the approach to determining health risks dependent on air quality standards60.
There have been other articles with contradictory findings, for instance, a study from Canada claimed that higher temperatures were associated with an increase in the prevalence of schizophrenia61. Many researchers have looked at the association between temperature and schizophrenia in various regions, and a rise in the frequency of schizophrenia-related emergency hospital visits has been documented as a result of daily temperature shift13,62,63, suggesting the existence of a delayed effect26,64. A thorough study of the prevalence of schizophrenia by Saha et al.65 revealed an increasing trend for schizophrenia by increasing latitude, indicating that regional differences may exist in the impacts of temperature 10,66. However, a study in Taiwan's tropical environment discovered a relationship between air temperature and hospitalizations for schizophrenia, revealing that cold weather may be a risk factor for the development of schizophrenia67. Due to the lack of sufficient research in India, it is suggested to explore this association in future studies. In the majority of the studies15,18,26, data was gathered from one region which may not be generally applicable. The results may not valid for other countries/regions. The time series data of schizophrenia was generally small. A relatively small sample size was used in many studies51. Specific age ranges (like 20 to 59 years) demonstrated greater vulnerability to the emergence of schizophrenia that may be caused by the development of schizophrenia at a young age or a small sample size, further research is required in such cases15. Data fusion in smart city environments is also a difficult consideration in the collection and analysis of data from disparate data sources68. The biological mechanism/reason behind the mysterious relationship between pollution and schizophrenia needs to be investigated further, which is not the intention of this review study.
Scope for further research
External validity can be improved by including different cities. There is also a need for research that spans multiple cities. The biological reason behind the exposure-response relation is also a matter of further research. The variables suggested are the length of the illness, treatment status, smoking or other forms of tobacco consumption, academic history, profession, and birthplace. Individual living environments and situations are not difficult to consider. SSP in the occurrence of mental disorders46 has been less investigated. Hospital outpatient visits characteristics, such as location, age, gender, and number of schizophrenia cases on the day, are the major attributes considered for the association. Subgroup analyses of age, gender, and marital status are also common in the literature. In the study of traffic-related exposure to air pollution and symptoms of psychiatric disorders especially in children19, underlying genetic vulnerability also can be considered in the future. The findings 42 of Pedersen et al. on traffic-related exposures, which were not responsible for the urban-rural disparities in schizophrenia risk, need replication. Time series studies with at least 3 years of weather data are required51 in some studies. Sample distribution and more health impairments for review should be included. Potential confounders, including BMI, level of education, cigarette behaviors, and medical histories were not available in many of the investigations, which might have influenced the correlations between air pollutants and schizophrenia. Collection of this kind of co-founders is also a difficult task because of the non-availability of such data in digital form and the privacy of individuals. The lack of indications of the severity of the condition, such as repeated hospital admissions, may restrict the in-depth examination of contaminants' involvement. Future studies require the application of simulated modelling scenarios to test the health impacts of environmental change and to validate whether the same model may be used to forecast psychiatric admissions from air pollution69.
Although some authors considered other data mining techniques, such as time series association rules70, different statistical, and machine learning techniques71, these techniques have not gained popularity as much as regression, DLNM, and correlation techniques on this problem. Across all situations and all parameters, there is no universal superiority by one system. The output varies according to the nature of the response component, the sample size, the number of contaminants involved, and the frequency of the association/interaction between exposure and response. Neural networks can be used in future research to explore the biological mechanism behind this association and also to reveal more underlying relationships between pollution and schizophrenia49,72,73.
Conclusion
In this review study, the impact of pollution and climate on schizophrenia was explored as available from existing literature. Dependencies between factors that predict pollutant intensity and clinical outcomes were predicted by the researchers. DLNM-based models are leading in exploring this association. The majority of them were mainly from Chinese cities to study the lag effect of pollutants on schizophrenia. It was found that different weather variables especially temperature may contribute to the development of psychosis in schizophrenia patients, potentially raising their admission rates to psychiatric facilities. The pollutants like PM, NO2, and SO2 also had a lag effect on schizophrenia. Some age and sex groups displayed greater susceptibility than other groups to schizophrenia emergence, which may be affected by schizophrenia onset or limited sample size. It is important to look into the basic biological mechanisms that underpin the relationship between environmental variables and schizophrenia admissions. Time series association techniques and deep learning algorithms have not experimented on this problem. These techniques may reveal unexplored aspects of the exposure-response problem. Temperature and major pollutants were explored more and noise pollution-based studies are comparatively less on schizophrenia. Additional research into several cities in different countries is required to improve the external validity of the study, including individual living environments and situations. The majority of findings need replication to validate their findings in different regions and conditions. The primary analysis of Bangalore data found that the association between environmental variables and schizophrenia is completely valid for detailed research in Indian cities. Urban-rural differences in the mental health domain are another interesting area for further study.
In this paper, we evaluated Bangalore data and found that the relationships mentioned for Chinese cities are also applicable to Indian data. Thereby, the researchers ascertained the environmental-schizophrenia relationships applicable across the globe. In the process, a rudimentary DLNM model was applied to determine the lag effect of environmental variables on schizophrenia. The primary results could be improved by exploring better models and algorithms as part of future work.
Acknowledgment
Thanks are owed to the hospitalization data provided by Bangalore hospitals including Cadabam hospitals, People Tree Maarga hospital, and Spandana hospital, as well as central pollution control board (CPCB) of India for providing data access through website.
Funding
The author(s) received no financial support for the research or publication of this review.
Conflict of interest
The authors declare that there is no conflict interest.
This is an Open-Access article distributed in accordance with the terms of the Creative Commons Attribution (CC BY 4.0) license, which permits others to distribute, remix, adapt, and build upon this work for commercial use.
References
- IPCC. Global Warming of 1.5°C. 2018. Available from:https://www.ipcc.ch/site/assets/ uploads/sites/2/2019/06/SR15_Full_Report_High_Res.pdf. [Cited 09 September 2022]
2. Fernández-Arteaga V, Tovilla-Zárate CA, Fresán A, et al. Association between completed suicide and environmental temperature in a Mexican population, using the Knowledge Discovery in Database approach. Comput Methods Programs Biomed. 2016;135:219-24.
3. Sarsam SM, Al-Samarraie H, Ismail N, et al. A real-time biosurveillance mechanism for early-stage disease detection from microblogs: a case study of interconnection between emotional and climatic factors related to migraine disease. Netw Model Anal Health Inform Bioinform. 2020;9(1):1-14.
4. Crombie R, Clark C, Stansfeld SA. Environmental noise exposure, early biological risk and mental health in nine to ten year old children: a cross-sectional field study. Environ Health. 2011;10(1):39.
5. Guxens M, Sunyer J. A review of epidemiological studies on neuropsychological effects of air pollution. Swiss Med Wkly. 2012;142:13322.
6. Lim YH, Kim H, Kim JH, et al. Air pollution and symptoms of depression in elderly adults. Environ Health Perspect. 2012;120(7):1023-8.
7. YoussefAgha A, Jayawardene W, Lohrmann D, et al. Application of data mining techniques to predict allergy outbreaks among elementary school children. Journal of Communication and Computer. 2012;10(2013):451-60.
8. Zhai Q, Li L, Yuan Y, et al. Correlation analysis of air pollution and respiratory disease in City A. In: International Conference on Remote Sensing, Environment and Transportation Engineering. 2011 Jun 24-26; Nanjing, China.
9. Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388(10039):86–97.
10. Kanani Sadat Y, Karimipour F, Kanani Sadat A. Investigating the relation between prevalence of asthmatic allergy with the characteristics of the environment using association rule mining. International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences; 2014. p.169-74.
11. Fink P. Physical disorders associated with mental illness: A register investigation. Psychol Med. 1990;20(4):829-34.
12. Calderón-Garcidueñas L, Solt AC, Henríquez-Roldán C, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid β-42 and α-synuclein in children and young adults. J Toxicol Pathol . 2008;36(2):289-310.
13. Gupta S, Murray RM. The relationship of environmental temperature to the incidence and outcome of schizophrenia. Br J Psychiatry. 1992;160(6):788-92.
14. Lin JN, Yang FY, Sun WZ, et al. Using methods of time series data mining to recognize the influences of environmental factors on epileptic seizures. Comput Electr Eng. 2018;68:437-46.
15. Duan J, Cheng Q, Luo X, et al. Is the serious ambient air pollution associated with increased admissions for schizophrenia?. Sci Total Environ. 2018;644:14-9.
16. Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Gen Psychiatr. 2003;60(12):1187-92.
17. Hingane LS, Rupa Kumar K, Ramana Murty BV. Long-term trends of surface air temperature in India. Int J Climatol. 1985;5(5):521-8.
18. Wang S, Zhang X, Xie M, et al. Effect of increasing temperature on daily hospital admissions for schizophrenia in Hefei, China: a time-series analysis. Public Health. 2018;159:70-7.
19. Yolton K, Khoury JC, Burkle J, et al. Lifetime exposure to traffic-related air pollution and symptoms of depression and anxiety at age 12 years. Environ Res. 2019;173:199-206.
20. Indian Council of Medical Research (ICMR). Available from: http://vizhub.healthdata.org/gbd-compare/india. [Cited 28 July 2019]
21. Abe K. Seasonal fluctuation of psychiatric admissions, based on the data for 7 prefectures of japan for a 7. year-period 1955–1961, with a review of literature. Psychiatry Clin Neurosci. 1963;17(2):101-12.
22. Petersen WF, Milliken ME. The patient and the weather. Nature. 1937;139:90-1
23. Newbury JB, Arseneault L, Beevers S, et al. Association of air pollution exposure with psychotic experiences during adolescence. JAMA Psychiatry. 2019;76(6):614-23.
24. Roberts S, Arseneault L, Barratt B, et al. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019;272:8-17.
25. Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Statistics in Medicine. 2010;29(21):2224-34.
26. Qiu H, Tak-sun Yu I, Tse LA, et al. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure?. Circ Heart Fail. 2013;6(5):930-5.
27. Liang Z, Xu C, Cao Y, et al. The association between short-term ambient air pollution and daily outpatient visits for schizophrenia: a hospital-based study. Environmental Pollution. 2019;244:102-8.
28. Engemann K, Pedersen CB, Arge L, et al. Childhood exposure to green space–a novel risk-decreasing mechanism for schizophrenia?. Schizophr Res. 2018;199:142-8.
29. Cameletti M, Gomez-Rubio V, Blangiardo M. Bayesian modelling for spatially misaligned health and air pollution data through the INLA-SPDE approach. Spat Stat. 2019;31:100353.
30. Howe CG, Eckel SP, Habre R, et al. Association of prenatal exposure to ambient and traffic-related air pollution with newborn thyroid function: findings from the Children’s Health Study. JAMA Netw Open. 2018;1(5):e182172.
31. Klompmaker JO, Hoek G, Bloemsma LD, et al. Surrounding green, air pollution, traffic noise exposure and non-accidental and cause-specific mortality. Environment International. 2020;134: 105341.
32 Yokobayashi R, Miura T. Multidimensional data mining based on tensor model. In: International Conference on Artificial Intelligence and Knowledge Engineering (AIKE). 2018 Sep 26-28. Laguna Hills, CA, USA.
33. Strous RD, Pollack S, Robinson D, et al. Seasonal admission patterns in first episode psychosis, chronic schizophrenia, and non-schizophrenic psychoses. The Journal of Nervous and Mental Disease. 2001;189(9):642-4.
34. Lin Y, Zhou L, Xu J, et al. The impacts of air pollution on maternal stress during pregnancy. Sci Rep. 2017;7:40956.
35. Liu JJ, Wang F, Liu H, et al. Ambient fine particulate matter is associated with increased emergency ambulance dispatches for psychiatric emergencies. Environ Res. 2019;177:108611.
36. Xu LJ, Shen SQ, Li L, et al. A tensor product quasi-Poisson model for estimating health effects of multiple ambient pollutants on mortality. Environmental Health. 2019;18:38.
37. Pun VC, Manjourides J, Suh H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the NSHAP study. Environ Health Perspect. 2017;125(3):342-8.
38. Rendall R, Pereira A, Reis M. An extended comparison study of large scale datadriven prediction methods based on variable selection, latent variables, penalized regression and machine learning. Comput Chem Eng. 2016;38:1629-34.
39. Eguchi R, Onozuka D, Ikeda K, et al. The relationship between fine particulate matter (PM2.5) and schizophrenia severity. Int Arch Occup Environ Health. 2018;91(5):613-22.
40. Dzhambov A, Tilov B, Markevych I, et al. Residential road traffic noise and general mental health in youth: The role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Environment International. 2017;109:1-9.
41. Bai L, Yang J, Zhang Y, et al. Durational effect of particulate matter air pollution wave on hospital admissions for schizophrenia. Environ Res. 2020;187:109571.
42. Pedersen CB, Mortensen PB. Urbanization and traffic related exposures as risk factors for schizophrenia. BMC Psychiatry. 2006;6:2.
43. Oudin A, Åström DO, Asplund P, et al. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: a case-crossover study. Environmental Health. 2018;17:4.
44. De Winter JC, Gosling SD, Potter J. Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: A tutorial using simulations and empirical data. Psychol Methods. 2016;21(3): 273.
45. Shiloh R, Shapira A, Potchter O, et al. Effects of climate on admission rates of schizophrenia patients to psychiatric hospitals. Eur J Psychiatry. 2005;20(1):61-4.
46. Yackerson NS, Zilberman A, Todder D, et al. The influence of air-suspended particulate concentration on the incidence of suicide attempts and exacerbation of schizophrenia. Int J Biometeorol. 2014;58(1):61-7.
47. Pedersen CB, Raaschou-Nielsen O, Hertel O, et al. Air pollution from traffic and schizophrenia risk. Schizophr Res. 2004;66(1):83-5.
48. De-sheng ZH, Ping BA, Jian CH, et al. Association of schizophrenia onset with exposure to outdoor thermal comfort: effect modification by individual characteristics. Chinese Journal of Disease Control & Prevention. 2021;25(4):460-5.
49. Kiang R, Adimi F, Soika V, et al. Meteorological, environmental remote sensing and neural network analysis of the epidemiology of malaria transmission in Thailand. Geospat Health. 2006; 1(1):71-84.
50. Carney PA, Fitzgerald CT, Monaghan CE. Influence of climate on the prevalence of mania. Br J Psychiatry. 1988;152(6):820-3.
51. Pan R, Zhang X, Gao J, et al. Impacts of heat and cold on hospitalizations for schizophrenia in Hefei, China: an assessment of disease burden. Sci Total Environ. 2019;694:133582.
52. Gu S, Huang R, Yang J, et al. Exposure-lag-response association between sunlight and schizophrenia in Ningbo, China. Environ Pollut. 2019;247:285-92.
53. Mawson D, Smith A. Relative humidity and manic admissions in the London area. Br J Psychiatry. 1981;138(2):134-8.
54. Tiddi I. Explaining data patterns using background knowledge from Linked Data. In: Proceedings of the Doctoral Consortium co-located with 12th International Semantic Web Conference. 2013 Oct 20. Sydney, Australia.
55. Dzhambov AM, Markevych I, Tilov B, et al. Pathways linking residential noise and air pollution to mental ill-health in young adults. Environ Res. 2018;166:458-65.
56. Wright B, Peters E, Ettinger U, et al. Understanding noise stress-induced cognitive impairment in healthy adults and its implications for schizophrenia. Noise Health. 2014;16(70): 166-76.
57. Marcelis M, Takei N, van Os J. Urbanization and risk for schizophrenia: does the effect operate before or around the time of illness onset?. Psychol Med. 1999;29(5):1197-203.
58. Sandfort TG, De Graaf R, Bijl RV, et al. Same-sex sexual behavior and psychiatric disorders: Findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Gen Psychiatr 2001;58(1):85-91.
59. Lewis G, David A, Andréassson S, et al. Schizophrenia and city life. The Lancet. 1992;340(8812):137-40.
60. Gore RW, Deshpande DS. An approach for classification of health risks based on air quality levels. In: 1st International Conference on Intelligent Systems and Information Management (ICISIM). 2017 Oct 5-6. Aurangabad, India.
61. Wang X, Lavigne E, Ouellette-kuntz H, et al. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J Affect Disord. 2014;155:154-61.
62. Clarke M, Moran P, Keogh F, et al. Seasonal influences on admissions for affective disorder and schizophrenia in Ireland: a comparison of first and readmissions. Eur Psychiatry. 1999;14(5):251-5.
63. Trang PM, Rocklöv J, Giang KB, et al. Heatwaves and Hospital Admissions for Mental Disorders in Northern Vietnam. PLoS One. 2016;11(5):e0155609.
64. Ye X, Wolff R, Yu W, et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19-28.
65. Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS medicine. 2005;2(5):e141.
66. Shaner A, Miller G, Mintz J. Evidence of a latitudinal gradient in the age at onset of schizophrenia. Schizophr Res. 2007;94(1-3):58-63.
67. Sung TI, Chen MJ, Lin CY, et al. Relationship between mean daily ambient temperature range and hospital admissions for schizophrenia: results from a national cohort of psychiatric inpatients. Sci Total Environ. 2011;410:41-6.
68. Fotopoulou E, Zafeiropoulos A, Papaspyros D, et al. Linked data analytics in interdisciplinary studies: The health impact of air pollution in urban areas. IEEE Access. 2015;4:149-64.
69. Vitolo C, Scutari M, Ghalaieny M, et al. Modeling air pollution, climate, and health data using Bayesian Networks: A case study of the English regions. Earth Space Sci. 2018; 5(4):76-88.
70. Payus C, Sulaiman N, Shahani M, et al. Association rules of data mining application for respiratory illness by air pollution database. Int J Basic Appl Sci. 2013;13(3):11-6.
71. Lary DJ, Lary T, Sattler B. Using machine learning to estimate global PM2.5 for environmental health studies. Environ Health Insights. 2015;9(S1):5664.
72. Craven MW, Shavlik JW. Using neural networks for data mining. Future Gener Comput Syst. 1997;13(2-3):211-29.
73. Song Q, Zhao MR, Zhou XH, et al. Predicting gastrointestinal infection morbidity based on environmental pollutants: Deep learning versus traditional models. Ecol Indic. 2017; 82:76-81.
3. Sarsam SM, Al-Samarraie H, Ismail N, et al. A real-time biosurveillance mechanism for early-stage disease detection from microblogs: a case study of interconnection between emotional and climatic factors related to migraine disease. Netw Model Anal Health Inform Bioinform. 2020;9(1):1-14.
4. Crombie R, Clark C, Stansfeld SA. Environmental noise exposure, early biological risk and mental health in nine to ten year old children: a cross-sectional field study. Environ Health. 2011;10(1):39.
5. Guxens M, Sunyer J. A review of epidemiological studies on neuropsychological effects of air pollution. Swiss Med Wkly. 2012;142:13322.
6. Lim YH, Kim H, Kim JH, et al. Air pollution and symptoms of depression in elderly adults. Environ Health Perspect. 2012;120(7):1023-8.
7. YoussefAgha A, Jayawardene W, Lohrmann D, et al. Application of data mining techniques to predict allergy outbreaks among elementary school children. Journal of Communication and Computer. 2012;10(2013):451-60.
8. Zhai Q, Li L, Yuan Y, et al. Correlation analysis of air pollution and respiratory disease in City A. In: International Conference on Remote Sensing, Environment and Transportation Engineering. 2011 Jun 24-26; Nanjing, China.
9. Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet. 2016;388(10039):86–97.
10. Kanani Sadat Y, Karimipour F, Kanani Sadat A. Investigating the relation between prevalence of asthmatic allergy with the characteristics of the environment using association rule mining. International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences; 2014. p.169-74.
11. Fink P. Physical disorders associated with mental illness: A register investigation. Psychol Med. 1990;20(4):829-34.
12. Calderón-Garcidueñas L, Solt AC, Henríquez-Roldán C, et al. Long-term air pollution exposure is associated with neuroinflammation, an altered innate immune response, disruption of the blood-brain barrier, ultrafine particulate deposition, and accumulation of amyloid β-42 and α-synuclein in children and young adults. J Toxicol Pathol . 2008;36(2):289-310.
13. Gupta S, Murray RM. The relationship of environmental temperature to the incidence and outcome of schizophrenia. Br J Psychiatry. 1992;160(6):788-92.
14. Lin JN, Yang FY, Sun WZ, et al. Using methods of time series data mining to recognize the influences of environmental factors on epileptic seizures. Comput Electr Eng. 2018;68:437-46.
15. Duan J, Cheng Q, Luo X, et al. Is the serious ambient air pollution associated with increased admissions for schizophrenia?. Sci Total Environ. 2018;644:14-9.
16. Sullivan PF, Kendler KS, Neale MC. Schizophrenia as a complex trait: evidence from a meta-analysis of twin studies. Gen Psychiatr. 2003;60(12):1187-92.
17. Hingane LS, Rupa Kumar K, Ramana Murty BV. Long-term trends of surface air temperature in India. Int J Climatol. 1985;5(5):521-8.
18. Wang S, Zhang X, Xie M, et al. Effect of increasing temperature on daily hospital admissions for schizophrenia in Hefei, China: a time-series analysis. Public Health. 2018;159:70-7.
19. Yolton K, Khoury JC, Burkle J, et al. Lifetime exposure to traffic-related air pollution and symptoms of depression and anxiety at age 12 years. Environ Res. 2019;173:199-206.
20. Indian Council of Medical Research (ICMR). Available from: http://vizhub.healthdata.org/gbd-compare/india. [Cited 28 July 2019]
21. Abe K. Seasonal fluctuation of psychiatric admissions, based on the data for 7 prefectures of japan for a 7. year-period 1955–1961, with a review of literature. Psychiatry Clin Neurosci. 1963;17(2):101-12.
22. Petersen WF, Milliken ME. The patient and the weather. Nature. 1937;139:90-1
23. Newbury JB, Arseneault L, Beevers S, et al. Association of air pollution exposure with psychotic experiences during adolescence. JAMA Psychiatry. 2019;76(6):614-23.
24. Roberts S, Arseneault L, Barratt B, et al. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019;272:8-17.
25. Gasparrini A, Armstrong B, Kenward MG. Distributed lag non-linear models. Statistics in Medicine. 2010;29(21):2224-34.
26. Qiu H, Tak-sun Yu I, Tse LA, et al. Is greater temperature change within a day associated with increased emergency hospital admissions for heart failure?. Circ Heart Fail. 2013;6(5):930-5.
27. Liang Z, Xu C, Cao Y, et al. The association between short-term ambient air pollution and daily outpatient visits for schizophrenia: a hospital-based study. Environmental Pollution. 2019;244:102-8.
28. Engemann K, Pedersen CB, Arge L, et al. Childhood exposure to green space–a novel risk-decreasing mechanism for schizophrenia?. Schizophr Res. 2018;199:142-8.
29. Cameletti M, Gomez-Rubio V, Blangiardo M. Bayesian modelling for spatially misaligned health and air pollution data through the INLA-
30. Howe CG, Eckel SP, Habre R, et al. Association of prenatal exposure to ambient and traffic-related air pollution with newborn thyroid function: findings from the Children’s Health Study. JAMA Netw Open. 2018;1(5):e182172.
31. Klompmaker JO, Hoek G, Bloemsma LD, et al. Surrounding green, air pollution, traffic noise exposure and non-accidental and cause-specific mortality. Environment International. 2020;134: 105341.
32 Yokobayashi R, Miura T. Multidimensional data mining based on tensor model. In: International Conference on Artificial Intelligence and Knowledge Engineering (AIKE). 2018 Sep 26-28. Laguna Hills, CA, USA.
33. Strous RD, Pollack S, Robinson D, et al. Seasonal admission patterns in first episode psychosis, chronic schizophrenia, and non-schizophrenic psychoses. The Journal of Nervous and Mental Disease. 2001;189(9):642-4.
34. Lin Y, Zhou L, Xu J, et al. The impacts of air pollution on maternal stress during pregnancy. Sci Rep. 2017;7:40956.
35. Liu JJ, Wang F, Liu H, et al. Ambient fine particulate matter is associated with increased emergency ambulance dispatches for psychiatric emergencies. Environ Res. 2019;177:108611.
36. Xu LJ, Shen SQ, Li L, et al. A tensor product quasi-Poisson model for estimating health effects of multiple ambient pollutants on mortality. Environmental Health. 2019;18:38.
37. Pun VC, Manjourides J, Suh H. Association of ambient air pollution with depressive and anxiety symptoms in older adults: results from the NSHAP study. Environ Health Perspect. 2017;125(3):342-8.
38. Rendall R, Pereira A, Reis M. An extended comparison study of large scale datadriven prediction methods based on variable selection, latent variables, penalized regression and machine learning. Comput Chem Eng. 2016;38:1629-34.
39. Eguchi R, Onozuka D, Ikeda K, et al. The relationship between fine particulate matter (PM2.5) and schizophrenia severity. Int Arch Occup Environ Health. 2018;91(5):613-22.
40. Dzhambov A, Tilov B, Markevych I, et al. Residential road traffic noise and general mental health in youth: The role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Environment International. 2017;109:1-9.
41. Bai L, Yang J, Zhang Y, et al. Durational effect of particulate matter air pollution wave on hospital admissions for schizophrenia. Environ Res. 2020;187:109571.
42. Pedersen CB, Mortensen PB. Urbanization and traffic related exposures as risk factors for schizophrenia. BMC Psychiatry. 2006;6:2.
43. Oudin A, Åström DO, Asplund P, et al. The association between daily concentrations of air pollution and visits to a psychiatric emergency unit: a case-crossover study. Environmental Health. 2018;17:4.
44. De Winter JC, Gosling SD, Potter J. Comparing the Pearson and Spearman correlation coefficients across distributions and sample sizes: A tutorial using simulations and empirical data. Psychol Methods. 2016;21(3): 273.
45. Shiloh R, Shapira A, Potchter O, et al. Effects of climate on admission rates of schizophrenia patients to psychiatric hospitals. Eur J Psychiatry. 2005;20(1):61-4.
46. Yackerson NS, Zilberman A, Todder D, et al. The influence of air-suspended particulate concentration on the incidence of suicide attempts and exacerbation of schizophrenia. Int J Biometeorol. 2014;58(1):61-7.
47. Pedersen CB, Raaschou-Nielsen O, Hertel O, et al. Air pollution from traffic and schizophrenia risk. Schizophr Res. 2004;66(1):83-5.
48. De-sheng ZH, Ping BA, Jian CH, et al. Association of schizophrenia onset with exposure to outdoor thermal comfort: effect modification by individual characteristics. Chinese Journal of Disease Control & Prevention. 2021;25(4):460-5.
49. Kiang R, Adimi F, Soika V, et al. Meteorological, environmental remote sensing and neural network analysis of the epidemiology of malaria transmission in Thailand. Geospat Health. 2006; 1(1):71-84.
50. Carney PA, Fitzgerald CT, Monaghan CE. Influence of climate on the prevalence of mania. Br J Psychiatry. 1988;152(6):820-3.
51. Pan R, Zhang X, Gao J, et al. Impacts of heat and cold on hospitalizations for schizophrenia in Hefei, China: an assessment of disease burden. Sci Total Environ. 2019;694:133582.
52. Gu S, Huang R, Yang J, et al. Exposure-lag-response association between sunlight and schizophrenia in Ningbo, China. Environ Pollut. 2019;247:285-92.
53. Mawson D, Smith A. Relative humidity and manic admissions in the London area. Br J Psychiatry. 1981;138(2):134-8.
54. Tiddi I. Explaining data patterns using background knowledge from Linked Data. In: Proceedings of the Doctoral Consortium co-located with 12th International Semantic Web Conference. 2013 Oct 20. Sydney, Australia.
55. Dzhambov AM, Markevych I, Tilov B, et al. Pathways linking residential noise and air pollution to mental ill-health in young adults. Environ Res. 2018;166:458-65.
56. Wright B, Peters E, Ettinger U, et al. Understanding noise stress-induced cognitive impairment in healthy adults and its implications for schizophrenia. Noise Health. 2014;16(70): 166-76.
57. Marcelis M, Takei N, van Os J. Urbanization and risk for schizophrenia: does the effect operate before or around the time of illness onset?. Psychol Med. 1999;29(5):1197-203.
58. Sandfort TG, De Graaf R, Bijl RV, et al. Same-sex sexual behavior and psychiatric disorders: Findings from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). Gen Psychiatr 2001;58(1):85-91.
59. Lewis G, David A, Andréassson S, et al. Schizophrenia and city life. The Lancet. 1992;340(8812):137-40.
60. Gore RW, Deshpande DS. An approach for classification of health risks based on air quality levels. In: 1st International Conference on Intelligent Systems and Information Management (ICISIM). 2017 Oct 5-6. Aurangabad, India.
61. Wang X, Lavigne E, Ouellette-kuntz H, et al. Acute impacts of extreme temperature exposure on emergency room admissions related to mental and behavior disorders in Toronto, Canada. J Affect Disord. 2014;155:154-61.
62. Clarke M, Moran P, Keogh F, et al. Seasonal influences on admissions for affective disorder and schizophrenia in Ireland: a comparison of first and readmissions. Eur Psychiatry. 1999;14(5):251-5.
63. Trang PM, Rocklöv J, Giang KB, et al. Heatwaves and Hospital Admissions for Mental Disorders in Northern Vietnam. PLoS One. 2016;11(5):e0155609.
64. Ye X, Wolff R, Yu W, et al. Ambient temperature and morbidity: a review of epidemiological evidence. Environ Health Perspect. 2012;120(1):19-28.
65. Saha S, Chant D, Welham J, et al. A systematic review of the prevalence of schizophrenia. PLoS medicine. 2005;2(5):e141.
66. Shaner A, Miller G, Mintz J. Evidence of a latitudinal gradient in the age at onset of schizophrenia. Schizophr Res. 2007;94(1-3):58-63.
67. Sung TI, Chen MJ, Lin CY, et al. Relationship between mean daily ambient temperature range and hospital admissions for schizophrenia: results from a national cohort of psychiatric inpatients. Sci Total Environ. 2011;410:41-6.
68. Fotopoulou E, Zafeiropoulos A, Papaspyros D, et al. Linked data analytics in interdisciplinary studies: The health impact of air pollution in urban areas. IEEE Access. 2015;4:149-64.
69. Vitolo C, Scutari M, Ghalaieny M, et al. Modeling air pollution, climate, and health data using Bayesian Networks: A case study of the English regions. Earth Space Sci. 2018; 5(4):76-88.
70. Payus C, Sulaiman N, Shahani M, et al. Association rules of data mining application for respiratory illness by air pollution database. Int J Basic Appl Sci. 2013;13(3):11-6.
71. Lary DJ, Lary T, Sattler B. Using machine learning to estimate global PM2.5 for environmental health studies. Environ Health Insights. 2015;9(S1):5664.
72. Craven MW, Shavlik JW. Using neural networks for data mining. Future Gener Comput Syst. 1997;13(2-3):211-29.
73. Song Q, Zhao MR, Zhou XH, et al. Predicting gastrointestinal infection morbidity based on environmental pollutants: Deep learning versus traditional models. Ecol Indic. 2017; 82:76-81.
Type of Study: Narrative review |
Subject:
Environmental Health, Sciences, and Engineering
Received: 2022/09/27 | Accepted: 2022/11/20 | Published: 2022/12/25
Received: 2022/09/27 | Accepted: 2022/11/20 | Published: 2022/12/25
Send email to the article author
| Rights and permissions | |
 |
This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License. |